Frozen shoulder, also known as adhesive capsulitis, is a condition that can significantly limit your shoulder’s mobility and cause pain and discomfort. If you’re struggling with frozen shoulder, this is here to help you understand what’s happening, why it’s happening, and what you can do to manage it.
What is Frozen Shoulder?
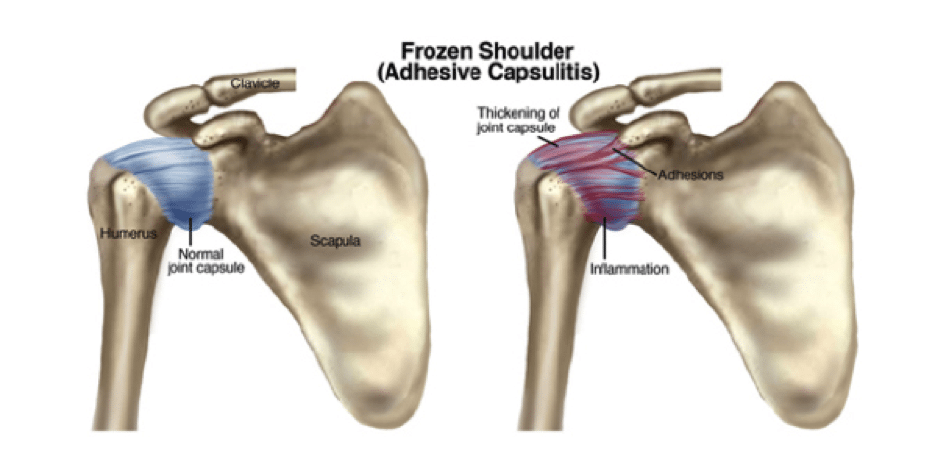
Frozen shoulder is an inflammatory condition where the shoulder joint becomes stiff, painful, and difficult to move. This happens because the capsule surrounding the shoulder joint becomes inflamed, thickened, and tight. It’s a slow process that can last for months or even years – this can all depend on how quickly you address the issue and what other conditions you may be suffering from.
- Definition: Frozen shoulder means your shoulder joint is “stuck” due to inflammation and scar tissue formation.
- Symptoms: Pain, stiffness, and difficulty moving your shoulder, especially with certain motions like reaching behind your back or lifting your arm.
What Causes Frozen Shoulder?
The exact cause isn’t always clear and it isn’t as simple as a one-size-fits-all diagnosis. It can be broken down into two categories: primary frozen shoulder and secondary frozen shoulder.
Primary Frozen Shoulder
- Happens without any obvious reason.
- More common in women aged 40-60, especially during menopause.
- Could be linked to changes in hormones or immune system function.
Secondary Frozen Shoulder
- Develops after another event or condition, such as:
- Injury or Surgery: Shoulder trauma or surgeries can lead to frozen shoulder if the joint isn’t moved enough afterward.
- Health Conditions: Diabetes, thyroid problems, and other medical issues can increase your risk.
What’s important to note is that while the causes may differ, both types of frozen shoulder follow the same progression – starting with pain, moving into stiffness, and eventually, a recovery phase.
Who is Most Likely to Get Frozen Shoulder?
Some groups are more likely to develop frozen shoulder than others:
- Women over 40: Hormonal changes, particularly during menopause, can increase risk.
- People with Diabetes: Frozen shoulder is more common in people with diabetes.
- After Injury or Surgery: Lack of movement after trauma or surgery can lead to stiffness.
- Other Medical Conditions: Thyroid problems and certain chronic illnesses can make you more susceptible.
Frozen Shoulder & Menopause – What’s the Connection?
Statistics (the not so fun ones – but the good to know ones)
- Menopause is where females have a major transition in their hormonal balance. There
- 47 million women worldwide enter the menopause transition annually
- >70% will experience some sort of musculoskeletal sign & symptoms
- 25% will be disabled by them through transition from perimenopause and post menopause
Why are women more susceptible
- Oestrogen is a natural anti-inflammatory and can help protect from chronic inflammatory diseases, oestrogens can also help shorten the pro-inflammatory phase and help resolve inflammation.
- Menopause is characterised by a significant drop in oestrogens therefore this decline starts to impact on all types of tissues (bone, muscle, tendons, ligaments, cartilage etc)
- Women also experience a reduction og 0.6% of muscle mass per year AFTER menopause, increasing the risk.
This is why it is so important taking care of our bodies in our younger years because our hormones don’t make things easier for us as we age.
Stages of Frozen Shoulder
Frozen shoulder progresses through three main stages, and each stage has its own challenges:
1. Freezing Stage (2-9 months)
- Symptoms: Gradual increase in shoulder pain that worsens over time. Movement becomes more restricted.
- What’s Happening: The shoulder capsule becomes inflamed and swollen.
- Focus: Managing pain and maintaining as much movement as possible without overdoing it.
2. Frozen Stage (4-12 months)
- Symptoms: Pain may decrease, but stiffness is the main issue. You’ll notice a significant loss of movement.
- What’s Happening: The inflammation subsides, but scar tissue forms, making the joint tight.
- Focus: Gentle strengthening and maintaining flexibility.
3. Thawing Stage (5-24 months)
- Symptoms: Gradual return of motion and less stiffness. Recovery happens slowly over time.
- What’s Happening: The scar tissue loosens, and the shoulder capsule begins to stretch.
- Focus: Gradually increasing movement and rebuilding strength.
Symptoms of Frozen Shoulder
Here’s how frozen shoulder typically presents:
- Pain: Often starts gradually and can worsen over time, especially at night.
- Stiffness: Makes it hard to perform everyday tasks like dressing or reaching overhead.
- Limited Movement: Both active (when you move your arm) and passive (when someone else moves it for you) range of motion are reduced.
- Common Movements Affected: Reaching behind your back, lifting your arm, and rotating your shoulder.
How is Frozen Shoulder Treated?
The good news is that frozen shoulder often resolves on its own over time, but treatment can help manage symptoms and speed up recovery.
1. Pain Management
- Over-the-counter pain medications like ibuprofen or acetaminophen can help.
- Heat therapy can reduce stiffness and make movement easier.
- In some cases, doctors may recommend corticosteroid injections to reduce inflammation.
2. Manual Therapy and Exercise
- Gentle stretching and mobility exercises can help maintain movement and reduce stiffness.
- Specific exercises tailored to the stage of frozen shoulder can make a big difference (see below).
3. Multidisciplinary Care
- Working with a physiotherapist, chiropractor, or other healthcare professional can provide additional relief through manual therapy or guided exercises.
Exercises for Frozen Shoulder
Tailoring exercises to the stage of frozen shoulder is key:
Freezing Stage (Painful Stage)
- Focus on gentle, pain-free movements:
- Pendulum swings: Let your arm hang and gently swing it in small circles.
- Wall crawls: Use your fingers to “crawl” up a wall, stopping if you feel pain.
- Stretching: Keep stretches short (1-5 seconds) and stay within your comfort zone.
Frozen Stage (Stiff Stage)
- Add strengthening exercises:
- Scapular retractions: Pull your shoulder blades back and down.
- Posterior capsule stretch: Gently pull your arm across your chest.
- Isometric exercises: Push against a wall or resistance band without moving your shoulder.
Thawing Stage (Recovery Stage)
- Gradually increase intensity:
- Doorway stretch: Place your arms on a doorway and gently lean forward.
- Strength training: Use light weights or resistance bands to rebuild shoulder strength.
- Functional movements: Focus on exercises that mimic daily tasks.
Visit our instagram page where we take you through our top stretching and strengthening exercises for frozen shoulder. Note these are for general use only, these videos should be used in conjunction with seeking medical advice from your trusted healthcare professional.
What You Can Do Today
If you’re experiencing frozen shoulder, here are some steps you can take:
- Start with gentle, pain-free movements to keep your shoulder active.
- Use heat therapy to reduce stiffness before exercising.
- Talk to a healthcare professional about a personalised plan of action to get you back doing what you love
- Remember, recovery takes time—be consistent and patient.
Final Thoughts: The Bottom Line
Frozen shoulder can be a frustrating and painful condition, but with the right approach, you can manage your symptoms and regain mobility over time. By staying active within your limits, working with healthcare professionals, and following a structured exercise plan, you’ll set yourself up for a successful recovery. Remember, progress may be slow, but it’s absolutely achievable.
If you are curious about how we can help, book an appointment with us! Our consult process is very thorough, involving a detailed history, a comprehensive examination and a tailored plan for what you are experiencing but also your lifestyle.
References:
Favejee, M. M., Huisstede, B. M. A., & Koes, B. W. (2011). Frozen shoulder: The effectiveness of conservative and surgical interventions—Systematic review. British Journal of Sports Medicine, 45(1), 49–56.
Hamed, D. H., Rodríguez-Pérez, C., Pruimboom, L., & Navarro-Ledesma, S. (2024). Relationship between metabolic profile, pain, and functionality in patients with frozen shoulder: A cross-sectional study. Healthcare, 12(23), 2444. https://doi.org/10.3390/healthcare12232444
Hand, C., Clipsham, K., Rees, J. L., & Carr, A. J. (2008). Long-term outcome of frozen shoulder. Journal of Shoulder and Elbow Surgery, 17(2), 231–236.
Kelley, M. J., McClure, P. W., & Leggin, B. G. (2009). Frozen shoulder: Evidence and a proposed model guiding rehabilitation. Journal of Orthopaedic & Sports Physical Therapy, 39(2), 135–148.
Massachusetts General Hospital. (n.d.). Rehabilitation protocol for frozen shoulder. Retrieved from https://www.massgeneral.org/assets/mgh/pdf/orthopaedics/sports-medicine/physical-therapy/rehabilitation-protocol-for-frozen-shoulder.pdf
Medical News Today. (n.d.). Frozen shoulder and menopause: Link and how to treat. Retrieved from https://www.medicalnewstoday.com/articles/frozen-shoulder-menopause#treatment
Pandey, V., & Madi, S. (2021). Clinical guidelines in the management of frozen shoulder: An update. Indian Journal of Orthopaedics, 55(2), 299–309. https://doi.org/10.1007/s43465-021-00351-3
Tashjian, R. Z. (2012). The effectiveness of nonoperative treatment for frozen shoulder: A systematic review. Clinical Journal of Sport Medicine, 22(2), 168–169. https://doi.org/10.1097/JSM.0b013e31824c2b01
Zhang, Z., Yan, Z., Chen, Y., & Ni, D. (2014). Intelligent frozen shoulder rehabilitation. IEEE Transactions on Neural Systems and Rehabilitation Engineering, 22(1), 39–47. https://doi.org/10.1109/TNSRE.2013.2285100


